Cases of a potentially deadly fungus have risen to an alarming rate — sparking a warning from the Centers for Disease Control and Prevention (CDC) that it is an "urgent threat" in a recent release about a new study published in the Annals of Internal Medicine.
Cases have soared nearly 200%, from 476 cases in 2019 to 1,471 in 2021 — and those cases were detected in over half of U.S. states, the CDC report found.
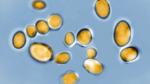
Candida auris or C. Auris is a fungus typically found in hospital settings and long-term care facilities.
It is a type of yeast.
CDC SAYS CASES OF LETHAL FUNGUS TRIPLED IN RECENT YEARS
It can cause severe infections and death in those who are immunocompromised or have underlying medical issues and indwelling devices, health experts told Fox News Digital.
The first case in the United States was back in 2013, with early cases found mainly in New York City and Chicago, according to the CDC published report.
"Candida auris is a strain of yeast that has been found in hospital settings," Dr. Frederick Davis, the associate chair of Emergency Medicine at Northwell Health on Long Island New York, told Fox News Digital.
The concern with this particular strain, he said, is that "many recent cases have been found to be resistant to commonly used medications to treat infection and in the limited number of cases have had a 30% to 60% mortality rate."
Davis was not involved in the CDC report.
He said the fungus "is usually not a threat to healthy individuals. In some people, it can reside on one’s skin and around the mouth or rectum and not cause any symptoms or concern. This is called asymptomatic colonization."
However, he said, "in chronically ill patients in health care facilities, it can enter the bloodstream through areas of open wound and lead to a symptomatic infection."
Those with an implanted device are more susceptible to this type of infection because the devices offer a surface for the fungus to colonize, the emergency medicine physician said.
POTENTIALLY DEADLY DRUG-RESISTANT FUNGUS SPREADING RAPIDLY IN US
Catheters could also be a source of transmission, he said, as they're usually inserted many times through the skin, where candida will reside.
"While most candida infections can present as a red patchy rash, the main concern is when candida gets into the bloodstream through an open wound. This will lead to fevers and look of sepsis."
Davis said this includes symptoms such as an increased heart rate and low blood pressure.
The other major concern about it, as health experts shared Fox News Digital, was that this type of fungus is resistant to many drugs that would be used to treat it.
"There are many types of antifungals; some of them work, and some of them don’t," said Aaron Glatt, M.D., chief of infectious diseases at Mount Sinai South Nassau Hospital on Long Island, New York.
"The concern is that these candida auris [infections] are already becoming resistant to many different types of antifungals available, so you are really limited in how you treat" them, he said.
"Bugs, fungi — they adapt," Glatt said.
He equated the ability of the fungus to adapt, much as a person adapts by putting on a sweater when it gets cold.
This adaptability of this fungus strain creates a threat to patients with underlying medical issues, he said.
"This is becoming more of a concern in very immunocompromised patients," he said.
The infectious disease expert said while this type of fungal infection is not something that healthy people typically need to be concerned about, they do need to be aware of preventing the spread of the fungus, especially in nursing home facilities, hospitals and long-term care units where there are vulnerable populations.
Precautions such as wearing gloves and gowns and properly washing hands could help limit the exposure and help prevent the spread of this fungus strain.
One possibility for the dramatic increase in cases of the fungus, according to the authors of the CDC report, could be due to decreased infection control measures during the pandemic, due to the strain that COVID-19 put on health care systems.
The strain resulted in shortages of staff and equipment, increased antimicrobial use and an increased disease severity of patients.